Global Health Supply Chains Face Unprecedented Stresses in Time of Unprecedented Need

A smooth-running global health supply chain is always essential, yet a once-in-a-century pandemic has challenged it like no other time.
Understanding those challenges and exploring ways to boost resilience were among the key topics of this year’s Global Health Supply Chain Summit, a three-day event that kicked off Nov. 17. Experts assembled — virtually, of course — across the globe to learn and share experiences about managing supply chains for and during COVID-19.
Keynote speakers were Vera Songwe, United Nations undersecretary-general and executive secretary of the Economic Commission for Africa; Muhammad Ali Pate, global director for health, nutrition, and population at the World Bank Group and director of the Global Financing Facility for Women, Children, and Adolescents; and Amer Daoudi, senior director of operation services for the World Food Programme, which won the 2020 Nobel Peace Prize.
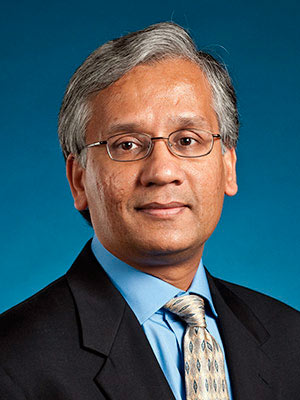
Conference co-chair Ravi Anupindi, professor of technology and operations at the University of Michigan Ross School of Business, discusses how those supply chains are faring with unprecedented stresses and what it might mean for distribution of coronavirus vaccines as promising progress is reported. His answers incorporate insights from members of the conference organizing committee.
What is the most striking effect of the pandemic on health supply chains? What products or people have been most affected? The least?
The most striking effect of the pandemic is how it has raised the base supply chain IQ of governments, health agencies, donors and the general public. The term “supply chain” before the pandemic was well known within operational and business circles but the pandemic has pushed the term into the global zeitgeist and has given all the stakeholders, whether local, regional, or global, a common and vivid reference point for its importance. Thus, supply chain discussions and transitions that prepandemic would have been expected to take years if not decades, are now arguably on an accelerated timeline.
Take, for example, how in the early months of the pandemic, the available global supply of health commodities related to COVID-19 was allocated along old fault lines of the “haves” and the “have nots.” In many cases, despite the global nature of the pandemic, some countries with local supply chains for commodities such as personal protective equipment and potential therapeutics, and some developed countries that could afford to overpay for such commodities, secured much of those commodities for their citizens — the haves — arguably at the expense of the welfare of citizens in countries lacking those resources the have-nots. But it turned out that even “the haves” needed lessons in supply chain management.
Having resources without paying attention to all the relevant supply chain connections needed to exploit them can still result in negative outcomes, as some found when they had reagent kits for COVID-19 testing but no cotton swabs for collecting samples from patients. And the “have-nots” have learned, or been reminded, that if you pay attention to the supply chains over which you do have some control, it can, with some providence, be leveraged to noteworthy accomplishments. For example, so far, Africa has generally avoided the worst of the pandemic partially due to their effective public health communication and leadership.
Like many Western nations, low- and middle-income countries (LMICs) also faced challenges in getting drugs and supplies needed for COVID-19, including PPEs, masks and tests. Lacking any purchasing leverage in a global marketplace that was already constrained for supply, those countries scrambled. However, the pandemic also had a broader impact on other aspects of health delivery as countries went into lockdowns, shutting down transport within and between countries as well as intercontinental transport. So movement of regular drugs for things like HIV, malaria or tuberculosis was severely constrained. Human resource capacity was also constrained as people had to work from home or maintain safe distances at work. Patients hesitated to visit overcrowded clinics and hospitals.
Now that we’re seeing some promising progress on vaccine development, what may be some supply chain challenges unique to vaccines for low- and middle-income countries?
Vaccines typically need to be kept cold or cool in order for them to maintain their potency, but some require freezing temperatures. This temperature requirement must be met along all sections of the supply chain. LMIC health supply chains typically handle vaccines that only need to be kept cold so COVID-19 vaccine candidates that require freezing temperatures, such as mRNA-based vaccines from Moderna and Pfizer/BioNTech, will pose operational challenges.
These challenges are expected to be temporary, as follow-on vaccines that do not have this ultra-cold requirement are expected to eventually become available. As a result, countries will need to focus on short-term solutions to these cold-chain challenges, such as using a third-party storage and distribution provider, but those may not always be available. Financing for COVID-19 vaccines will also pose a challenge for LMIC countries because of the high quantities of vaccines being contemplated and some expectations that these purchases will be annual at least in the short term.
The two major challenges as we move ahead will be access to sufficient quantities of vaccines and financing the procurement and distribution of vaccines. With global constrained supply and weak purchasing power, will these countries get sufficient vaccines to cover at least essential workers? More broadly, the world needs to consider what “a fair and equitable allocation” means if we assume that every life has equal value.
With a theme around resiliency, you and the other organizers clearly want to emphasize ways to get control of — or at least a handle on — the management of supply chains in the midst of a pandemic. Can you provide an example of a new technology or design that’s helped overcome obstacles?
It is difficult at this time to credibly speak about overcoming obstacles with much of the world still within the grips of the pandemic. There is also the reality that much of what works during a supply chain shock are the consequence of process, structures, and people that were put in place before and in expectation of some shock. The majority of what we expect to hear at the conference is about the consequences of these experiences and decisions made before the pandemic that attendees are now finding have had the desired or serendipitous effect. To be sure, there will be situations involving new steps that have been taken after the pandemic started, but invariably those efforts will build on preparations that began prior to the pandemic and whose implementation timeline has been accelerated.
So, again, it is early to give concrete examples but here is what I have been hearing: Health systems in countries that already had been working with the private sector were able to respond faster and better. Private sector has the agility to step in to ramp up capacity and ensure delivery. Another strategy that was already being put in place in some countries prepandemic was to use eCommerce-type models for chronic medicine delivery. For instance, instead of a patient coming to a clinic to get their next medicine refill, say for HIV, because the prescription was still valid, medicines could be mailed to them. Such innovation helps reduce congestion in clinics, which became an imperative during the pandemic. The pandemic has also made countries, at least in sub-Saharan Africa, realize the value of regional collaboration to pool their purchasing power to get better access to PPEs, masks and more.
What else is important to add or amplify about the state of global health supply?
The benefits of experience with and preparation for shocks like the COVID-19 pandemic cannot be overstated. Another reason suggested for Africa’s and some Asian countries’ ability to weather the COVID-19 storm is the benefits of recent outbreaks and epidemics, from which much has been learned. And in activities where developing countries do not have much experience, such as vaccine manufacturing in Africa, there are significant opportunities to learn from the experiences of others.
Many health technologies in the developed world which now hold great promise for addressing current and future health issues in developing countries have advanced beyond their basic research origins over the recent decades and are now very close to achieving their potential. This includes biotech for new therapeutics and vaccines, and the technology to manufacture these therapeutics. In supply chain management, advances in information technology hold promise for improving the visibility into where commodities are in the supply chain and for providing the information needed for improved decision making.
The cost curve for many of these advances increasingly favor adoption by developing countries given the benefits and reduction in their costs that have accrued from the experiences in developed countries using these technologies. Developing countries will increasingly find themselves able to leapfrog into technologies and processes similar to those of developing countries and with diligence, in some cases, outpace them.